PCOS. The Gorilla in the room.
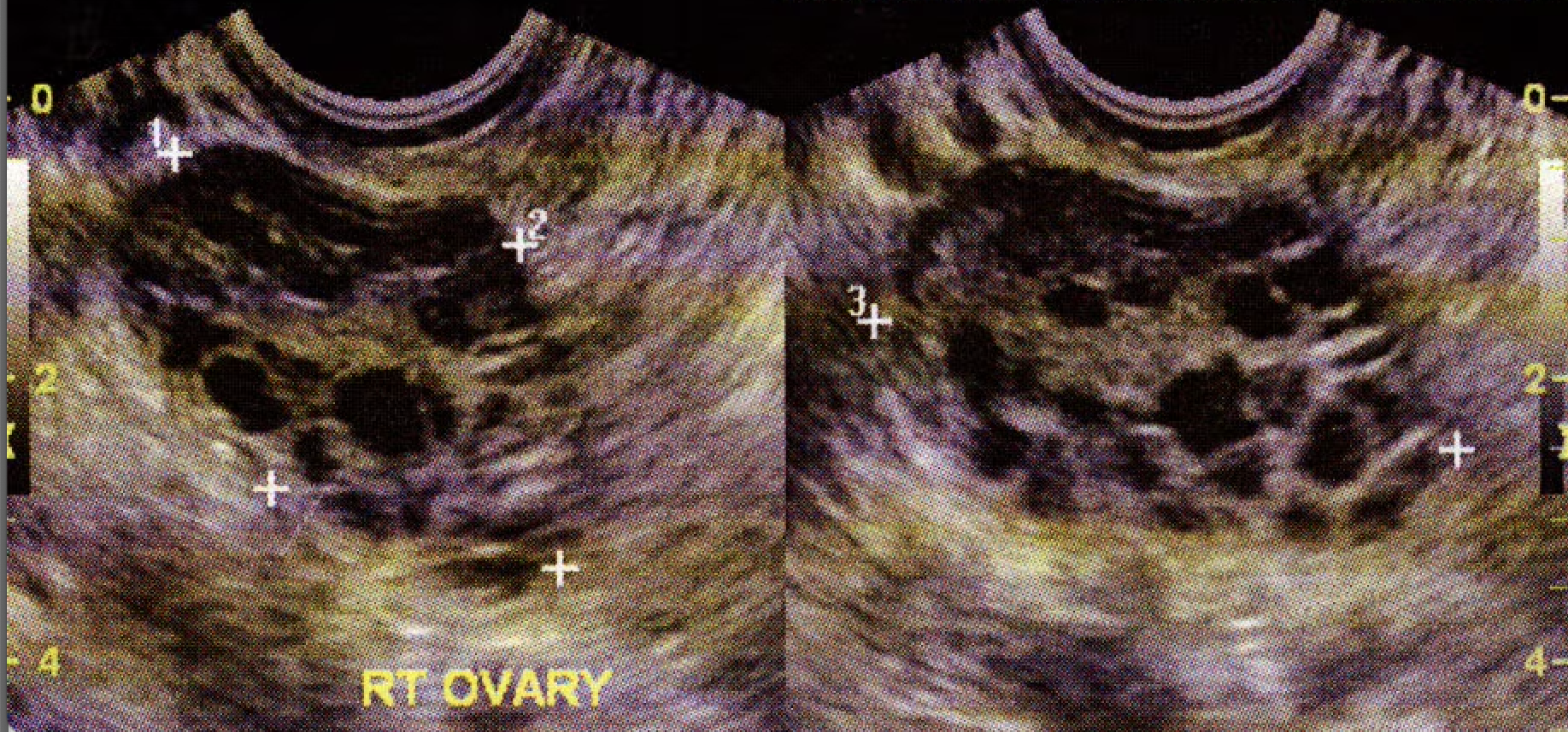
Polycystic Ovaries on Ultrasound
There’s a gorilla in the room — and it’s PCOS. Millions of women have it, but most are told to ‘just lose weight’ or ‘wait it out.’
One of the most common gynecologic problems for women in the U.S. is also one of the least acknowledged — and often one of the most frustrating to deal with: Polycystic Ovary Syndrome (PCOS).
It affects millions of women, yet we still don’t fully understand it. And to make matters worse, a lot of what’s out there about PCOS is either oversimplified, outdated, or just plain wrong.
What Causes PCOS?
The short answer: we don’t know exactly.
There’s definitely a family connection, but no single gene has been identified. One thing we do know for sure — it’s not caused by obesity.
A big piece of the puzzle seems to involve insulin resistance. When the body’s insulin levels run high, it can lower something called SHBG (sex hormone binding globulin). That leads to higher levels of testosterone, which then makes your body produce even more testosterone. (You can see where this is going — a vicious cycle that feeds itself.)
Insulin also interacts with the brain, increasing appetite and making it even harder to maintain balance. So no, it’s not just about “eating right” — there’s real biology at work here.
Ruling Out Other Causes
We always have to make sure it’s actually PCOS and not something else. There are a few rarer conditions that can look very similar, like:
Adrenal or ovarian tumors
Adult-onset congenital adrenal hyperplasia
Cushing’s syndrome
Pituitary tumors (like a prolactinoma)
This is why getting a thorough evaluation really matters.
How PCOS Shows Up
Most women come in because of period problems — irregular, heavy, or sometimes completely missing cycles. But that’s rarely the only thing going on.
Other common symptoms include:
Infertility or trouble getting pregnant
Hair growth in unwanted places (chin, chest, etc.)
Acne or oily skin
Thinning hair on the scalp
Weight gain or difficulty losing weight
Sleep apnea, fatigue, or non-alcoholic fatty liver disease
And PCOS isn’t just about what’s happening now — it can affect your long-term health too. Women with PCOS have higher risks of:
Diabetes (especially after age 30 — almost 8x higher risk!)
Endometrial cancer
Heart disease and cholesterol problems
Depression
And possibly breast cancer
It’s also common to see family histories of early heart disease and diabetes in PCOS patients. The more irregular your cycles, the higher the risk for long-term metabolic and cardiovascular issues.
Why Fertility Can Be Harder
The main reason women with PCOS struggle with fertility is something called anovulation — meaning they don’t release an egg regularly. No egg = no pregnancy opportunity.
But that doesn’t mean pregnancy is impossible. Many women with PCOS conceive naturally or with just a little help.
What We Do About It
Treatment really depends on whether you’re trying to get pregnant right now or not.
If You’re Not Trying to Conceive
We focus on managing symptoms and reducing long-term risks.
Lifestyle changes matter, but not in a “just lose weight” kind of way.
We’re talking about realistic, sustainable changes — a high-fiber, low glycemic index diet and about 150 minutes a week of moderate to intense exercise. I usually recommend roughly 70% cardio and 30% strength training.
Medications that help:
Metformin: Helps your body respond to insulin better, reduces your diabetes risk, and may help with weight control.
GLP-1 analogs (Ozempic, Wegovy, Victoza, etc.): These have honestly been game changers for PCOS. They can dramatically improve weight management, help balance hormones, and give women back a sense of control.
Cycle control:
Hormonal options like birth control pills or IUDs help regulate or suppress periods, reduce heavy bleeding, improve acne and unwanted hair growth, and lower your risk for endometrial cancer.
For skin and hair issues:
There are medications that can help, but truthfully, laser hair removal is still the gold standard for long-term improvement.
Screening matters:
We also check regularly for diabetes, cholesterol issues, high blood pressure, and cancer risk factors — because prevention is power.
If You’re Trying to Conceive
We shift gears toward optimizing your body’s natural balance and helping you ovulate.
Overall optimization: Getting your general health in check helps any fertility treatment work better.
Ovulation induction: We can use medications to “nudge” your body into releasing an egg. The most common are Clomid and Femara (the latter is often better tolerated and more effective).
Fun fact: these treatments slightly increase your chances of having twins!
Final Thoughts
PCOS is incredibly common, but it’s not “normal,” and it’s definitely not something you just have to live with.
At Calhoun Women’s Center, we help women understand what’s going on, take back control of their health, and actually feel better. Whether your main concern is fertility, cycles, or just feeling like yourself again — there’s help, and we’d love to be part of that process.
📞 Call 706-509-8251 to schedule an appointment.